High density lipoprotein
High-density lipoprotein (HDL) is a complex of lipids and proteins that is particularly high in the protein component and that binds with cholesterol and triglycerides and transports them in the circulatory system. The cholesterol bound to HDL also is referred to as good cholesterol because it is thought to have beneficial actions.
HDL is the smallest and densest of the five major groups of lipid-protein complexes known as lipoproteins that enable certain water-insoluble lipids, like cholesterol, to be transported within the water-based blood stream. The other major categories of lipoproteins are chylomicrons, very low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and low-density lipoprotein (LDL).
There are a number of lifestyle changes that people can make to raise the levels of this "good cholesterol." Among these are aerobic exercise, loss of weight, lowering intake of saturated fats and alcohol, and adding dietary fiber.
Overview
Cholesterol plays a central role in many biochemical processes. It is a major constituent in the cell membranes of animals and serves as a precursor of important hormones and other substances. Cholesterol is the principal sterol in all vertebrate cells (McGraw-Hill 2002).
Cholesterol, however, is insoluble in blood and is transported in the circulatory system bound to one of the varieties of lipoprotein. These lipoproteins are spherical particles that have an exterior composed mainly of water-soluble proteins. They bind to lipids like cholesterol and triglycerides and allow them to be transported within the water-based blood stream. High-density lipoproteins (HDLs) are the smallest of the lipoprotein particles. In healthy individuals, about thirty percent of blood cholesterol is carried by HDL (AHA 2008).
In recent years, the term "good cholesterol," or "healthy cholesterol," is used to refer to cholesterol contained in HDL, thought to have beneficial actions, while the term "bad cholesterol" has been used to refer to cholesterol contained in LDL (low-density lipoprotein), which is thought to have harmful actions. It is hypothesized that HDL can remove cholesterol from atheroma within arteries and transport it back to the liver for excretion or re-utilization—which is the main reason why HDL-bound cholesterol is sometimes referred to as good cholesterol or HDL-C. A high level of HDL-C seems to protect against cardiovascular diseases, and low HDL cholesterol levels (less than 40 mg/dL) increase the risk for heart disease (AHA 2008). When measuring cholesterol, any contained in HDL particles is considered as protection to the body's cardiovascular health, in contrast to "bad" LDL cholesterol.
Structure and function
HDL are the densest of the lipoprotein particles because they contain the highest proportion of protein. Their most abundant apolipoproteins are apo A-I and apo A-II (BCM).
The liver synthesizes these lipoproteins as complexes of apolipoproteins and phospholipid, which resemble cholesterol-free flattened spherical lipoprotein particles. They are capable of picking up cholesterol, carried internally, from cells by interaction with the ATP Binding Cassette Transporter A1 (ABCA1). A plasma enzyme called lecithin-cholesterol acyltransferase (LCAT) converts the free cholesterol into cholesteryl ester (a more hydrophobic form of cholesterol), which is then sequestered into the core of the lipoprotein particle, eventually making the newly synthesized HDL spherical. They increase in size as they circulate through the bloodstream and incorporate more cholesterol and phospholipid molecules from cells and other lipoproteins, for example by the interaction with the ABCG1 transporter and the phospholipid transport protein (PLTP).
HDLs deliver their cholesterol mostly to the liver or steroidogenic organs such as adrenals, ovary, and testes by direct and indirect pathways. The direct HDL removal pathways involve HDL receptors such as scavenger receptor BI (SR-BI), which mediate the selective uptake of cholesterol from HDL. In humans, the probably most relevant pathway is the indirect one, which is mediated by cholesteryl ester transfer protein (CETP). This protein exchanges triglycerides of VLDL against cholesteryl esters of HDL. As the result, VLDL are processed to LDLs, which are removed from the circulation by the LDL receptor pathway. The triglycerides are not stable in HDL, but degraded by hepatic lipase so that only small HDL particles are left, which restart the uptake of cholesterol from cells.
The cholesterol delivered to the liver is excreted into the bile and hence intestine either directly or indirectly after conversion into bile acids. Delivery of HDL cholesterol to adrenals, ovaries, and testes are important for the synthesis of steroid hormones.
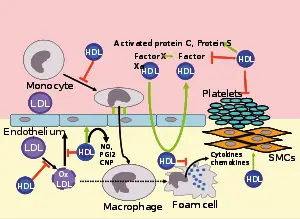
Several steps in the metabolism of HDL can contribute to the transport of cholesterol from lipid laden macrophages of atherosclerotic arteries, termed foam cells to the liver for secretion into the bile. This pathway has been termed reverse cholesterol transport and is considered as the classical protective function of HDL towards atherosclerosis.
However, HDL carries many lipid and protein species, many of which have very low concentrations but are biologically very active. For example, HDL and their protein and lipid constituents help to inhibit oxidation, inflammation, activation of the endothelium, coagulation, or platelet aggregation. All these properties may contribute to the ability of HDL to protect from atherosclerosis, and it is not yet known what is most important.
In the stress response, serum amyloid A, which is one of the acute phase proteins and an apolipoprotein, is under the stimulation of cytokines (IL-1, IL-6) and cortisol produced in the adrenal cortex and carried to the damaged tissue incorporated into HDL particles. At the inflammation site, it attracts and activates leukocytes. In chronic inflammations, its deposition in the tissues manifests itself as amyloidosis.
It has been postulated that the concentration of large HDL particles more accurately reflects protective action, as opposed to the concentration of total HDL particles (Kwiterovich 2000). This ratio of large HDL to total HDL particles varies widely and is only measured by more sophisticated lipoprotein assays using either electrophoresis (the original method developed in the 1970s), or newer NMR spectroscopy methods, developed in the 1990s.
A link has been shown between level of HDL and onset of dementia. Those with high HDL were less likely to have dementia (Nagourney 2008). Low HDL-C in late-middle age has also been associated with memory loss (Singh-Manoux et al. 2008).
Epidemiology
Men tend to have noticeably lower HDL levels, with smaller size and lower cholesterol content, than women. Men also have an increased incidence of atherosclerotic heart disease.
Epidemiological studies have shown that high concentrations of HDL (over 60 mg/dL) have protective value against cardiovascular diseases such as ischemic stroke and myocardial infarction. Low concentrations of HDL (below 40 mg/dL for men, below 50 mg/dL for women) increase the risk for atherosclerotic diseases.
Data from the landmark Framingham Heart Study showed that for a given level of LDL, the risk of heart disease increases 10-fold as the HDL varies from high to low. Conversely, for a fixed level of HDL, the risk increases 3-fold as LDL varies from low to high.
Even people with very low LDL levels are exposed to some increased risk if their HDL levels are not high enough (Barter et al. 2007).
Recommended range
The American Heart Association, NIH and NCEP provides a set of guidelines for male fasting HDL levels and risk for heart disease.
| Level mg/dL | Level mmol/L | Interpretation |
| <40 | <1.03 | Low HDL cholesterol, heightened risk for heart disease, <50 is the value for women |
| 40–59 | 1.03–1.52 | Medium HDL level |
| >60 | >1.55 | High HDL level, optimal condition considered protective against heart disease |
Measuring HDL
Many laboratories use a two-step method for measuring HDL: chemical precipitation of lipoproteins containing apoprotein B, then calculating HDL as cholesterol remaining in the supernate (Lin et al. 1998). However, there also are direct methods (MDRTC). Labs use the routine dextran sulfate-Mg2+ precipitation method with ultracentrifugation/dextran sulfate-Mg2+ precipitation as a reference method (Bairaktari et al. 1999). HPLC can be used (Okazaki et al. 1997).
Subfractions (HDL-2C, HDL-3C) can be measured (Hirano et al. 2008) and have clinical significance.
Raising HDL
Drugs
Pharmacological therapy to increase the level of HDL cholesterol includes use of fibrates and niacin. Consumption of pharmacologic doses of niacin can increase HDL levels by 10–30 percent (Medscape 2004), and it is the most powerful agent currently available to increase HDL-cholesterol (Chapman et al. 2004; Roze et al. 2007). A randomized clinical trial demonstrated that such treatments can significantly reduce atherosclerosis progression and cardiovascular events (Drexel 2008). However, niacin products sold as "no-flush," in other words not having side effects such as "niacin flush," do not contain free nicotinic acid and are therefore ineffective at raising HDL, while products sold as "sustained release" may contain free nicotinic acid, but "some brands are hepatotoxic;" therefore the recommended form of niacin for raising HDL is the cheapest, immediate release preparation (Myers et al. 2003).
In contrast, while the use of statins is effective against high levels of LDL cholesterol, it has little or no effect in raising HDL cholesterol (Brewer 2005).
Torcetrapib, a promising new drug developed by Pfizer to raise HDL by inhibition of cholesteryl ester transfer protein (CETP), was terminated after a greater percentage of patients treated with torcetrapib-Lipitor combination died compared with patients treated with Lipitor alone. Merck is currently researching a similar molecule called anacetrapib.
Diet and lifestyle
Certain changes in lifestyle can have a positive impact on raising HDL levels (Fogoros 2007):
- Aerobic exercise (Spate-Douglas and Keyser 1999)
- Weight loss
- Smoking cessation
- Removing trans fatty acids from the diet
- One drink of alcohol a day or less yields higher HDL-C levels, more so in women than men. HDL transports cholesterol to the liver and cholesterol is known to have a protective effect on the cell membrane. It is likely that this reflects the liver's need for more cholesterol to protect itself from the alcohol (Weidner et al. 2008).
- Adding soluble fiber to diet
- Using supplements such as omega 3 fish oil (CCHVI)
- Limiting intake of saturated fats
ReferencesISBN links support NWE through referral fees
- American Heart Association (AHA). 2008. LDL and HDL cholesterol: What's bad and what's good? American Heart Association. Retrieved January 23, 2009.
- Bairaktari, E., M. Elisaf, A. Katsaraki, V. Tsimihodimos, A. D. Tselepis, K. C. Siamopoulos, and O. Tsolas. 1999. Homogeneous HDL-cholesterol assay versus ultracentrifugation/dextran sulfate-Mg2+ precipitation and dextran sulfate-Mg2+ precipitation in healthy population and in hemodialysis patients. Clinical Biochemistry 32(5): 339-346. Retrieved January 23, 2009.
- Barter, P., A. M. Gotto, J. C. LaRosa, et al. 2007. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. New England Journal of Medicine 357: 1301-1310. Retrieved January 23, 2009.
- Baylor College of Medicine (BCM). n.d. Apolipoprotein. Lipids Online (Baylor College of Medicine). Retrieved January 23, 2009.
- Brewer, H. B. 2005. Raising HDL-cholesterol and reducing cardiovascular risk. Medscape. Retrieved January 23, 2009.
- Chapman, M., G. Assmann, J. Fruchart, J. Shepherd, and C. Sirtori. 2004. Raising high-density lipoprotein cholesterol with reduction of cardiovascular risk: The role of nicotinic acid—a position paper developed by the European Consensus Panel on HDL-C. Cur Med Res Opin. 20(8):1253-68. PMID 15324528.
- Cleveland Clinic Heart and Vascular Institute (CCHVI). n.d. What are omega-3 fatty acids? Cleveland Clinic Heart and Vascular Institute. Retrieved January 23, 2009.
- Drexel, H. 2008. Reducing risk by raising HDL-cholesterol: The evidence. European Heart Journal Supplements 8(Suppl F): F23-F29. Retrieved January 23, 2009.
- Fogoros, R. N. 2007. Raising your HDL levels: Increasing the GOOD cholesterol. About.com. Retrieved January 23, 2009.
- Hirano, T., K. Nohtomi, S. Koba, A. Muroi, and Y. Ito. 2008. A simple and precise method for measuring HDL-cholesterol subfractions by a single precipitation followed by homogenous HDL-cholesterol assay. Journal of Lipid Research 49: 1130-1136. Retrieved January 23, 2009.
- Kwiterovich, P. O. 2000. The metabolic pathways of high-density lipoprotein, low-density lipoprotein, and triglycerides: A current review. Am J Cardiol 86(suppl):5L.
- Lin, M.-J., C. Hoke, and B. Ettinger. 1998. Evaluation of homogeneous high-density lipoprotein cholesterol assay on a BM/Hitachi 747–200 analyzer. Clinical Chemistry. 44: 1050-1052. Retrieved January 23, 2009.
- McGraw-Hill. 2002. McGraw-Hill Encyclopedia of Science and Technology. New York: McGraw-Hill. ISBN 0079136656.
- Medscape. 2004. Clinical strategies to elevate HDL. Medscape Cardiology 8(1). Retrieved January 23, 2009.
- Michigan Diabetes Research and Training Center (MDRTC). n.d. Lipid measurement fact sheet. University of Michigan. Retrieved January 23, 2009.
- Meyers, C. D., C. Molly, S. Park, and J. D. Brunzell. 2003. Varying cost and free nicotinic acid content in over-the-counter niacin preparations for dyslipidemia. Annals of Internal Medicine 139 (12): 996-1002. Retrieved January 23, 2009.
- Nagourney, E. 2008. Aging: Good cholesterol, good memory. New York Times July 1st, 2008. Retrieved January 23, 2009.
- Okazaki, M., K. Sasamoto, T. Muramatsu, and S. Hosaki. 1997. Evaluation of precipitation and direct methods for HDL-cholesterol assay by HPLC. Clin Chem 43(10): 1885-1890.
- Roze, S., J. Ferrières, E. Bruckert, E. Van Ganse, M. J. Chapman, D. Liens, and C. Renaudin. 2007. Cost-effectiveness of raising HDL cholesterol by adding prolonged-release nicotinic acid to statin therapy in the secondary prevention setting: A French perspective. International Journal of Clinical Practice 61(11): 1805-1811.
- Singh-Manoux, A., D. Gimeno, M. Kivimaki, E. Brunner, and M. G. Marmot. 2008. LLow HDL cholesterol is a risk factor for deficit and decline in memory in midlife: The Whitehall II study. Arterioscler Thromb Vasc Biol. 28(8): 1556-62. Retrieved January 23, 2009.
- Spate-Douglas, T., and R. E. Keyser. 1999. Exercise intensity: Its effect on the high-density lipoprotein profile. Arch Phys Med Rehabil 80: 691-695. Retrieved January 23, 2009. PMID 10378497. Retrieved January 23,2009.
- Weidner, G., S. L. Connor, M. A. Chesney, J. W. Burns, W. E. Connor, J. D. Matarazzo, and N. R. Mendell. 1991. Sex differences in high-density lipoprotein cholesterol among low-level alcohol consumers. Circulation 83: 176-180. Retrieved January 23, 2009.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.